RETINAL VEIN OCCULSION
What is Retinal Vein Occulsion?
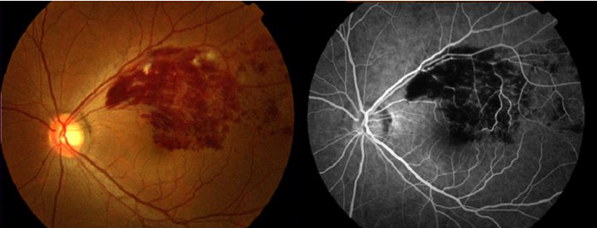
Retinal vein occlusion is a condition where veins of the retina become blocked, resulting in leakage of blood and plasma (fluid from the bloodstream) into the retinal tissue. The bleeding (haemorrhage) and swelling (oedema) in the retina can cause symptoms such as blurred, distorted or loss of central vision.
Disruption of the blood supply to the retinal tissues can also result in a lack of oxygen and nutrition and cause permanent damage, such as loss of retinal circulation (ischaemia) or development of abnormal new blood vessels (neovascularisation). These abnormal new blood vessels unfortunately are fragile and have a tendency to bleed, which can result in vitreous haemorrhage, scarring of the retinal tissues, tractional retinal detachment and greater visual loss. In addition, if the vessels develop in the drainage angle of the eye, a severe form of glaucoma can also occur (rubeotic or neovascular glaucoma).
Who is More Likely to Develop Retinal Vein Occlusion?
Retinal vein occlusion typically occurs in individuals greater than 50 years of age and is more common in patients with high blood pressure, diabetes, glaucoma, cardiovascular diseases, blood clotting disorders, or other inflammatory conditions.
What are the Different Types of Vein Occlusions?
There are two different types:
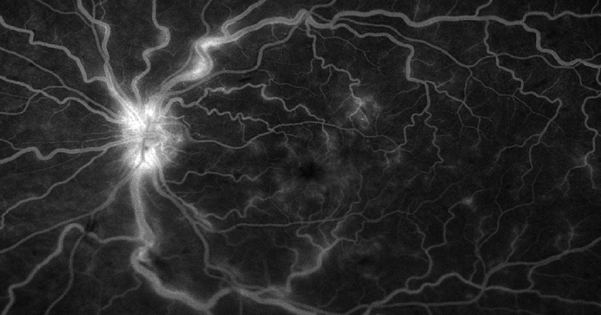
- Central retinal vein occlusion (CRVO) if the blockage occurs in the main vein leaving the optic nerve of the eye.
- Branch retinal vein occlusion (BRVO) if the blockage occurs at one of the branches before reaching the main vein at the optic nerve.
What Tests Do I Need to Have?
When retinal vein occlusion is suspected, patients would need to undergo investigations such as a fluorescein angiogram and an OCT scan to determine the site and severity of the blockage as well as identifying the area of ischaemia (poor circulation). As retinal vein occlusion is often associated with macular oedema (swelling), an OCT scan is very valuable in evaluating the degree of fluid accumulation and monitoring treatment efficacy.
What is the Treatment?
Intravitreal injections with Eylea (anti-VEGF drugs) have been found to be highly effective in treating macular oedema and improving vision in many cases. Regular treatments and follow-ups will be required. Laser can also be applied to areas of ischaemia. Any risk factors such as hypertension, hyperlipidaemia should also be treated.
