CATARACT SURGERY BRISBANE
What is Cataract Surgery?
Considering to have cataract surgery but worried if it is safe?
Cataract surgery is a safe and routine procedure. It is usually performed as a day surgery procedure under monitored local anaesthesia called twilight sedation.
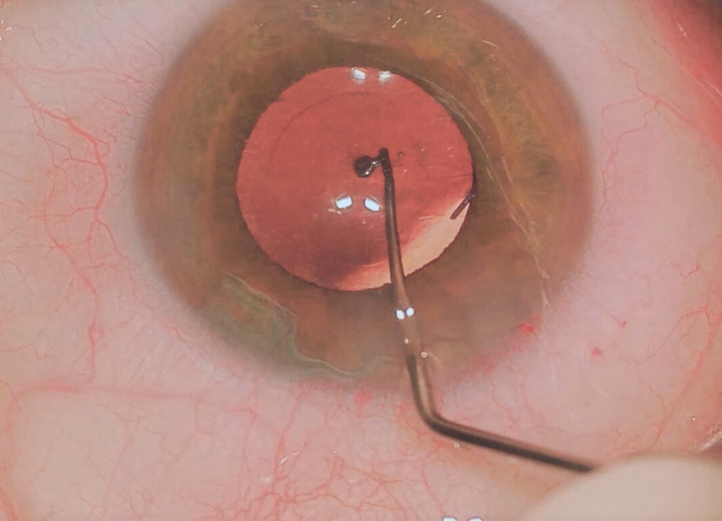
Cataract surgery involves the use of phacoemulsification which is an ultrasound probe connected to a highly advanced phaco machine. This removes the cataract through a very small incision in the cornea. Once the cataract has been removed, a permanent artificial intraocular lens (IOL) is injected into the eye. The small incision usually seals itself or a suture may be required.
How Do I Decide Whether to Have Cataract Surgery?
Cataract formation is a slow process. It may take years for the cataract to start interfering with your vision. As cataract progresses, your vision may reduce and you may notice glare and difficulties with daily activities such as reading and driving.
We will examine your eyes and determine how much the cataract is contributing to your reduced vision. Dr Lee will discuss the benefits and risks of proceeding with cataract surgery and answer your questions or concerns. Dr Lee will also discuss with you the type of intraocular lenses that will most suit your visual needs.
Pre-operative Assessment
Pre-operative assessment for your cataract surgery includes an examination of your general health, medications, and allergies. These factors will affect the decision to proceed with surgery, the type of anaesthesia required, and the recovery process. Prior to surgery, we will perform a comprehensive eye examination including an OCT scan and/or perimetry field test. A-scan biometry with the IOLMaster will be performed to calculate the required power of the intraocular lens to be inserted during the operation.
Prior to surgery, it is important to advise us if you are taking any anticoagulation drugs. These include aspirin, Warfarin, Eliquis, Pradaxa, Plavix or prostate medications such as Duodart and Tamsulosin. They may interfere with pupil dilation during surgery. If you are diabetic, it is important to advise of your medications, particularly if you are on insulin, SGLT2 inhibitors such as Janumet or GLP-1 inhibitors such as Ozempic.

Premium Lens Selection
There are many intraocular lens options available. Your occupation, lifestyle preferences, and daily activities determine your visual needs and the type of lens best suited to accommodate your requirement.
- Extended depth of field (EDOF) lenses: The newer EDOF lenses are designed to improve mid-range vision. They do not have the concentric rings of the multifocal lens types. This provides an extended focus from arm’s length to distance vision. Many of our patients are happy with their excellent vision with the EDOF lenses. Many also reduce their spectacle dependency, only using glasses for very fine near tasks.
- Toric lenses: We select the appropriate toric lenses if you have significant astigmatism. Correcting your astigmatism optimizes your vision and may reduce your need for glasses.
- Mono-focal lenses: This provides clear vision at a fixed distance, either at distance or near. This can be used as a combination involving monovision where one lens is focused for distance and one for near.
- Multi-focal lenses: Whilst this aims to provide clear vision at all distances, there may be side-effects such as rings or haloes around lights.
Post-operative Care
Following surgery, it is important to follow the post-operative instructions to maximize your visual recovery. The eyes should be kept clean and dry. Take care while showering to avoid getting water in the eye for the first two weeks. A plastic eye shield should be worn at night for at least the first week following surgery to prevent any trauma to the eye.
Activities such as swimming, bending, heavy lifting and high impact exercise should be avoided for a month. You may perform your usual daily activities after a few days as long as care and hygiene are maintained. Eye drops will be required during the post-operative period. This will minimize risks of infection, reduce inflammation, and/or control the intraocular pressure. Very rarely, tablets may be required to control the pressure. Artificial tears such as Systane, Optive, Hyloforte may be used. We usually refer you back to your local optometrist 6-8 weeks after surgery.
Cataract surgery is a safe procedure and complications are rare. However, symptoms of reduced vision, redness or pain require urgent attention as they may indicate complications such as infection, inflammation or development of retinal problems such as retinal detachment.
Do you have questions or concerns about your eye health or a specific eye condition? To discuss, please contact City Eye Centre for more information.
