CORNEAL TRANSPLANTATION / GRAFT
Corneal transplantation aims to replace the hazy cornea with a clear donor cornea, with the aim of providing improved vision and a stable eye surface.
Corneal transplantation techniques have developed over recent years and there are now several options with improved vision potential and faster recovery with less complications. Partial-thickness transplantation to transplant the anterior cornea such as deep anterior lamellar keratoplasty (DALK) has been used in keratoconus. Endothelial transplantation has improved recovery and success in cases of endothelial disease such as in Fuchs dystrophy. Full-thickness corneal transplantation, is still used in certain cases that require full-thickness layer transplantation such as in dense corneal scars.
What is involved in a corneal transplantation?
Corneal graft surgery requires a donor cornea from another person who has kindly donated their tissue for transplantation. All materials are to be cleared by the Queensland Eye Bank for transmissible diseases such as Hepatitis B & C, HIV, syphilis. Corneal surgery can be performed under a local or general anaesthetic.
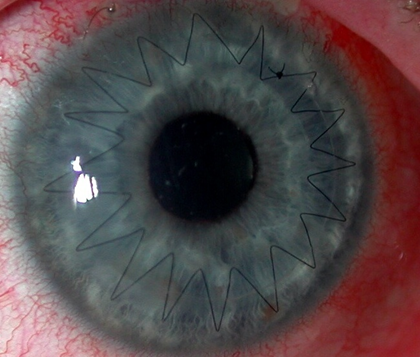
In cases of full thickness corneal graft, a round blade called a trephine is used to remove the patient’s diseased cornea. The donor cornea is then harvested from the donated eye and stitched into the patient’s eye with a very fine Nylon suture, one tenth of a human hair. This suture usually remains for 12 months after which the suture will need to be removed. In partial thickness corneal transplant, only the anterior layers are removed and replaced so there is faster recovery and less risk of rejection. In endothelial transplant only the endothelial (deep) layer is replaced and a gas bubble is used to position the new endothelium in place.
What happens after the transplantation?
Most corneal graft patients take 2-3 weeks off post-operation, depending on the type of occupation they perform. Bending, heavy lifting and straining should be avoided in the first two weeks. Swimming should also be avoided whilst on the steroid drops, as there is an increased risk of eye infection. The visual recovery is gradual over the first few months. The final visual outcome will occur usually about 12 months, and when the sutures if they were used are removed at one year. Most patients will require glasses and occasionally contact lenses to achieve best vision.
Two types of medications will be required, a steroid and an antibiotic, after the graft surgery. Initially you will be using it quite frequently, eg every 2-3 hours during the day for the first month. The drops are then tapered according to recovery over the next two months. Some patients may require long-term eye drops, particularly if they have had previous graft surgery.
What are the possible complications?
Success rate of graft surgery is very good, however with any surgery there are potential risks. These include infection, bleeding and reduced vision. Specific to graft surgery there is the risk of rejection of the corneal graft, as it is tissue from a donor. If this occurs, treatment in the form of drops need to be commenced as soon as possible. Generally, it is possible to reverse the rejection, however if rejection recurs multiple times, it can result in failure of the graft. In this circumstance the graft will need to be replaced. Astigmatism (irregular curvature of the cornea) occurs in all grafts to a varying degree and this can be corrected with glasses or contact lenses. When the suture is removed after 12 months, prescription of the glasses and contact lenses will change and an update in refraction would be required.
